“False Alarm” Appendix
“It’s a red hot appendix. Get down to the hospital right away and we will take it out.” It all sounds so simple. Indeed it would be a great blessing if it were actually as simple as this sounds. Long experience, however, has taught many of us who practice medicine to make haste slowly in order that full justice may be done both to our patient and to our own professional reputation. We must realize the possibility of a “false alarm” appendix. In other words, symptoms which might lead one to suspect appendicitis, while imaginary in themselves, might lead to a very real operation.
So, too, good old-fashioned constipation has cost many a man his appendix—along with whatever it takes to pay for an operation, nurses’ care, and a hospital bill. Just a case of mistaken identity, however, as the gangster courteously explained, upon finding that he had beaten up the wrong man. Rather sorry comfort to the victim to know that his injuries were not really intended for him. So, too, if you are subjected to an operation for the removal of your appendix without “good and sufficient reasons,” as the lawyers say. Any honest surgeon will tell you of many cases in which the removed appendix was found to be normal. Of course, to save his face, the surgeon refers to it (when speaking to the family) as a chronically inflamed appendix.
How, then, do such mistakes come about? Any case of constipation can be developed into what looks like an undoubted case of appendicitis by doing the wrong things. In the presence of obstinate constipation, positively the worst thing in the world is to take a cathartic. The more violent the cathartic, the more potent the purgative, the more likely one is to develop pain and nausea and even vomiting—all of which symptoms are sufficient to make an alert surgeon suspect appendicitis.
Naturally, the cathartic or purgative is irritating to the membrane of the colon, since many cathartic substances act by virtue of their irritant qualities. The irritation of the colon membrane induces cramps and gas formation. The gas, along with fecal masses in the colon, gives rise to pain and more or less tenderness on pressure. The presence of an abnormal amount of gas in the intestines, together with the continued absorption of the putrefactive products of retained feces, all contribute to a sense of biliousness or nausea. So you see we can evolve an almost perfect picture of an acute appendicitis from what started out as a simple case of common constipation.
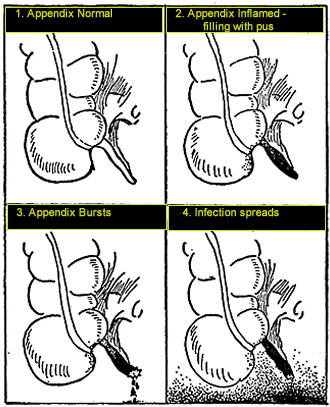
However, it is only fair to add that if the above procedure is persisted in, or if the patient has for any reason a lowered resistance, actual inflammation of the appendix may occur. Then the appendix constitutes a serious menace. If washroom advice is now followed, or if the spell of the advertisements continues, the patient will make still further attempts to “keep regular” or to try this or that highly recommended “bowel cleanser.” The end result of all this may be a ruptured appendix, a very sick patient, and a much wiser though sadder man—if he lives.
Most cases, however, are not quite so fearsome as that just described. A little common sense and a carefully given enema will dispel a majority of so-called appendicitis cases. The reference to common sense implies the avoidance of cathartics in cases of constipation associated with abdominal pain, fever, vomiting, or persistent nausea.
If a simple enema gives no relief, and distress is felt in the abdomen, the wisest course is to call a doctor. If, following a careful examination, the doctor decides that the patient would be safer in a hospital, by all means listen to his suggestion—following it may mean the life of a loved one. Always remember that if the case is seen early enough, properly diagnosed, and carefully handled, there is nothing to fear. With kindly guidance of a conscientious doctor, the patient can be well on the road to recovery within a week.
Fig. 7. Diagram showing progress of appendicitis
Who ever heard of a person having an attack of appendicitis after his appendix had been removed? Well I, for one, have, and no doubt intestinal specialists elsewhere have encountered the same strange state of affairs. It is just this experience that leads me to the question, “But is it appendicitis?”
In solving this health mystery story, let us return to the original attack of false-alarm appendicitis. We find the patient describing the usual signs of appendicitis, pain or ache over the right side of his abdomen, or, as he says, “pain in the stomach.” When the doctor who examined him at that time pressed the painful spot, it was found to be acutely tender. Moreover, the whole abdomen felt somewhat bloated and distressed. Because of this gas he felt sick to his stomach. All in all, the doctor felt sure it was appendicitis. He operated.
Much to his surprise, he found only an innocent-looking little appendix apparently minding its own business. Imagine the surgeon’s embarrassment, and picture how he kept mumbling to himself as he finished the operation in anticipation of telling the family, “Chronically inflamed appendix—not serious, but better out than in”—and so forth. All proving that, if you keep saying anything long enough, you will come to believe it.
However, specialists in intestinal ailments know the answer. The trouble never was appendicitis but a form of colitis associated with spasm. In cases of colitis such as I have just mentioned, it must be evident that, since the entire colon was involved, little good could be expected from the surgical removal of that small portion of it known as the appendix.
A large percentage of patients who have come to me for the treatment of colitis have had their appendixes removed some years prior to the discovery that they had colitis. Many others have had what had been diagnosed from time to time as intestinal influenza.
Needless to say, there is a strong likelihood that in many of these cases the appendix was not the basic cause of the condition which finally resulted in its removal. So far as the diagnosis of “intestinal influenza” is concerned, it should be known that even among doctors it is a very vague term. Most specialists in intestinal diseases recognize it as an unsuspected colitis, confused with the general condition known as influenza.
For more than ten years in my writings addressed both to the profession and to the laity, I have been crying out for the recognition of the facts mentioned above. I am sure that I have saved more than one person from unnecessary operations and other wrong treatments.
It is most gratifying to note that in a recent issue of the Journal of the American Medical Association, Dr. Alvarez, well-known specialist at the Mayo Clinic, says, in reviewing his experience with nearly four hundred patients upon whom the appendix operation was performed wrote: “The patient is supposed to have everything to gain and nothing to lose. Would to God this were true! . . . actually 60 of the 255 patients . . . were decidedly the worse for the operation . . . only two were cured.”
“It would seem,” concludes Dr. Alvarez, “that true chronic appendicitis, instead of being regarded as the commonest abdominal disease, should be thought of as one of the rarest.”
Of late years when in the course of examining a patient, I notice a small neat scar over the region of the appendix, I immediately suspect that the symptoms he now complains of were the very same symptoms he had before his appendix were removed. In most cases, my suspicion is verified by the patient. The colitis he is suffering from at the present time is precisely the same ailment he was suffering from when it was considered necessary to remove his appendix.
Through the natural processes of nervous reaction, it warns a person of the disorder existing in the colon. In response to that warning, a few inconsequential inches are nipped off and the patient is asked to believe that’s all there is, brother, that’s all. Well the colon has a different idea and in time reasserts its discontent. Eventually, some patient doctor, by thorough examination, reveals to the patient the fact that the colitis is the ailment which he has had all during the time he was being treated for appendicitis.
When the truth is known, perhaps the colon mumbles to itself: “Who’s looney now?” Written By: J. F. Montague, M.D., Continue Reading: “Blow-out Pockets” in the Colon: Diverticulosis

No Comments